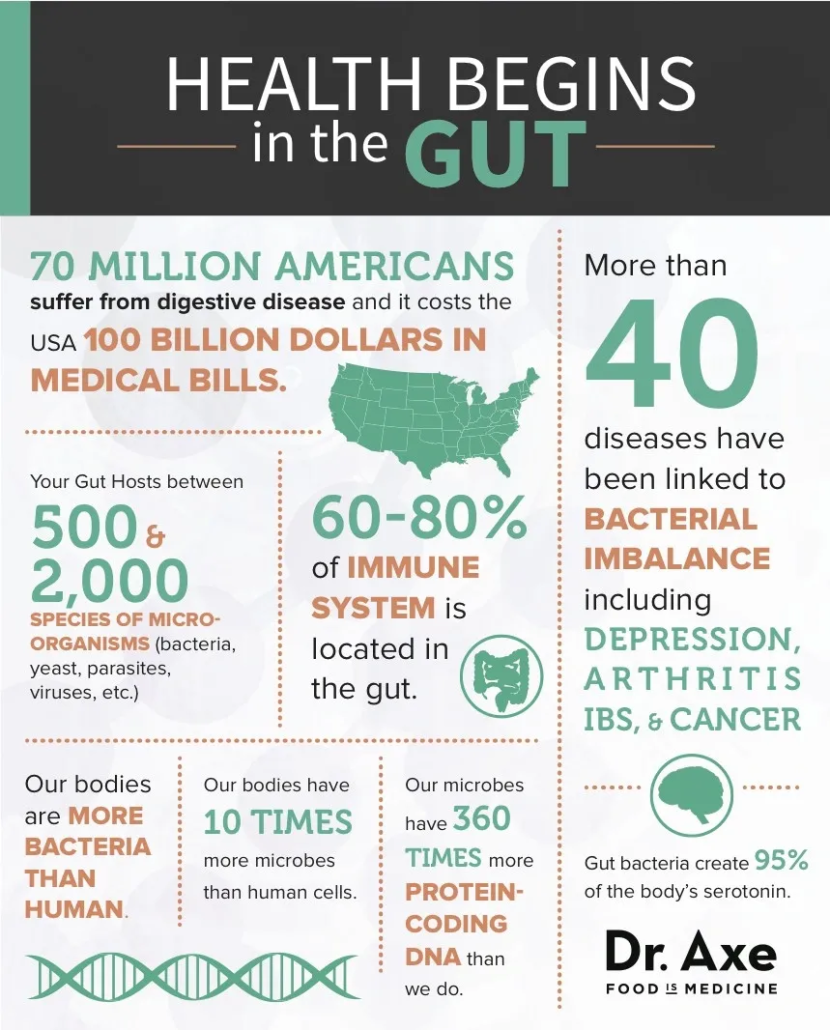
The gut microbiota consists of the collection of microbes within the intestine, previously considered of little influence from a mental health perspective, but now regarded as a “virtual organ” weighing up to 1.5 kg in the adult intestine and producing molecules of primary importance for brain function and psychological well‐being1.There are more bacteria in the human intestine than there are human cells in the body, and we feed these bacteria, while in turn they play a fundamental role in maintaining our overall health. The large intestine functions like a fermenter producing a variety of molecules, including most common neurotransmitters such as gamma‐aminobutyric acid (GABA) and serotonin, the serotonin precursor tryptophan, and the short chain fatty acids butyrate, propionate and acetate2.
There are a variety of mechanisms enabling the gut microbes to communicate with the brain. These include the vagus nerve, short chain fatty acids, tryptophan and cytokines3. Certain microbes can only act centrally when the vagus nerve is intact, and can no longer do so following vagotomy. Previously, tryptophan was viewed as entirely of dietary origin, while now it has been established that it is also synthesized by Bifidobacteria and enters the bloodstream, becoming available for brain entry and subsequent serotonin synthesis.
The gut microbiota has been implicated in a wide variety of neurological and psychiatric disorders, including Parkinson’s disease, multiple sclerosis, depression, anxiety disorders and autism4. Much of what we know regarding the importance of gut microbes for brain function has been derived from studying germ‐free animals, which do not have a gut microbiota. Such animals have an altered central serotonergic system, decreased dendritic spines in various brain regions, lower levels of trophic factors, along with abnormal neuron formation from progenitor cells in the hippocampus, altered myelination patterns in prefrontal cortex, and a defective blood‐brain barrier.
Until relatively recently, the importance of the gut‐brain‐microbiota axis as a fundamental component of the stress response has largely been ignored. O’Mahony et al5 studied the gut microbiota in a maternal separation model of depression in rats. They reported an elevation in corticosterone in such animals, together with an increase in pro‐inflammatory cytokines and a decrease in the diversity of gut microbes.
The fecal microbiota was then sequenced in a depression study6. Forty‐six patients with depression and 30 healthy controls were recruited. High‐throughput pyrosequencing showed increased faecal bacterial diversity in those currently depressed, but not in a group who had responded to treatment. This suggests that increased diversity is a state rather than trait marker for depression. Despite the extensive inter‐individual variability, levels of several predominant genera differed between depressed patients and controls. The former had increased levels of Enterobacteriaceae and Alistipes, but reduced levels of Faecalibacterium.
In a study conducted at APC Microbiome Ireland, depressed patients had elevated cortisol output together with decreased faecal microbial richness. When rats were given a humanized microbiota from depressed patients, as opposed to healthy controls, they developed a depressive phenotype from both a behavioral and immune perspective7.
Thus, there is increasing evidence that some psychiatric disorders such as depression may be associated with a gut dysbiosis, a microbial imbalance.
Several studies have investigated the microbiome composition in patients with bipolar disorder8. The first published study involved 115 patients and reported decreased levels of Faecalibacterium. This finding was replicated in an Austrian study of 32 patients. However, a Danish study of 113 patients with newly‐diagnosed bipolar disorder compared to unaffected first‐degree relatives and healthy individuals found no differences in Faecalibacterium, while Flavonifractor, a bacterial genus that may induce oxidative stress and inflammation, was associated with the disorder.
Interestingly, two recent clinical trials have demonstrated a beneficial effect of adjunctive psychobiotics in patients with bipolar disorder. One was an uncontrolled pilot study which reported cognitive improvements in 20 remitted individuals following three months consumption of nine different strains of Lactobacillus or Bifidobacterium. The second was a randomized controlled trial involving 66 patients who had recently been hospitalized for mania. After discharge, these patients were randomly assigned to receive 24 weeks of an adjunctive Lactobacillus/Bifidobacterium combination or placebo. Re‐hospitalization rates were significantly lower in those individuals who were taking the psychobiotic. Thus, preliminary data support the view that probiotics of the Lactobacillus and Bifidobacterium genera hold therapeutic potential in bipolar disorder.
Unlike genes in human cells, we can readily change genes in our microbiota by altering diet. There is increasing evidence that a poor quality diet may bring about the altered microbiota observed in mood disorders. Narrowing of dietary diversity with reduced intake of essential nutrients can reduce the availability of substrates for specific microbial growth and this may contribute to the intestinal dysbiosis of depression and other psychiatric disorders.
Over recent decades, dietary patterns in the West and elsewhere have undergone major compositional changes, with increased intakes of red meat, high fat foods, and refined sugars. This “Westernization” of diets results in dysbiosis, which may at least partially contribute to the increasing incidence of chronic inflammatory disorders, such as depression. The Mediterranean diet is associated with lower rates of depression and impacts optimally on the gut microbiota. Preliminary evidence indicates that such a diet may have antidepressant effects.
Individuals with depression or vulnerability to depression should be encouraged to enhance a plant‐based diet with a high content of grains and fibres9. A decreased consumption of red meat, especially of processed meat, and a regular intake of fish and fermented foods, is optimal from a mental health perspective. The intake of refined sugars should be restricted.
Incorporating the gut microbiota in our studies of stress‐related psychiatric illnesses expands the range of therapeutic targets, not only for pharmacological interventions, but also for nutritional ones. This may be one of the missing links that have restricted therapeutic advances in psychiatry during the past decades.